HeaRTNovation
3D-printed Polyetheretherketone (PEEK) Osteosynthesis Plates for Simple Mandibular Fractures
TECHNOLOGY GENERATOR
Rentor Y. Cafino, M.D.
Zamboanga City Medical Center
THE PROBLEM
Mandibular fractures are a significant concern in craniofacial trauma, as the mandible is the most frequently fractured bone in the face. The primary causes of these fractures include vehicular accidents, physical trauma, falls, or sports injuries. The increased frequency of road accidents, particularly in urban areas, has further contributed to the rising incidence of mandibular fractures.
The clinical management of mandibular fractures is inherently complex, requiring precise anatomical reduction, stable fixation, and the restoration of both function and occlusion. Traditional surgical approaches—typically involving metallic osteosynthesis plates—have been effective but are not without limitations. These include extended operative times, the potential for soft tissue irritation, infection, stress shielding, and complications such as malocclusion or non-union. Moreover, the rigidity of conventional titanium implants may not mimic the biomechanical properties of bone, potentially affecting long-term healing and functionality. These challenges underscore the need for innovative, patient-specific, and biomechanically compatible solutions to improve clinical outcomes and reduce recovery times.
THE SOLUTION

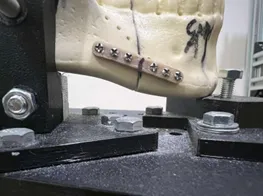
Polyetheretherketone (PEEK) is a high-performance thermoplastic increasingly recognized as a viable alternative to titanium in craniomaxillofacial (CMF) surgery due to its biomechanical compatibility with human cortical bone. With an elastic modulus that closely mirrors the bone, PEEK helps reduce stress shielding and supports improved clinical outcomes. This study, spearheaded by the Zamboanga City Medical Center, focuses on the biomechanical evaluation of in-house 3D printed PEEK osteosynthesis plates as a cost-effective and timely solution for mandibular fracture fixation. Traditionally, custom implants are procured from third-party manufacturers, resulting in long waiting times and high costs. In contrast, in-house manufacturing using advanced CAD/CAM systems and additive manufacturing allows for the rapid production of patient-specific implants, precisely tailored to individual anatomy. This approach not only reduces surgical delays and expenses but also enhances surgical precision, promotes faster recovery, and improves both functional and aesthetic results.
TECHNOLOGY DEVELOPMENT STATUS
The technology is currently at Technology Readiness Level (TRL) 4, indicating validation of the concept in a laboratory setting with completed biomechanical testing. It is currently being utilized as a hospital-based manufacturing model.
MARKET VIABILITY
The innovation is at Investment Readiness Level (IRL) 3, where concept validation is complete, and development is progressing toward product-market fit. The target market includes government and private hospitals, specialty surgical centers, and biomedical manufacturers with interests in patient-specific implants and trauma care.
CURRENT NEEDS
The project team is actively seeking partners, particularly clinical collaborators, and biomedical engineers, for further development, scaling, and validation of the technology. Interest is also extended to distributors and institutional adopters willing to co-develop clinical protocols and support regulatory clearances.
CONTACT DETAILS
Dr. Maria Monique Theresita M. Soliven
OIC Unit Head
Advanced Manufacturing in Medicine – ADMAM3D (formerly ENT-HNS Medical Makerspace)
Zamboanga City Medical Center
admam3d@gmail.com